Obesity: Reviving the Promise of Leptin
The History of Leptin
- Discovered by Douglas Coleman (The Jackson Laboratory, Bar Harbor, Maine)
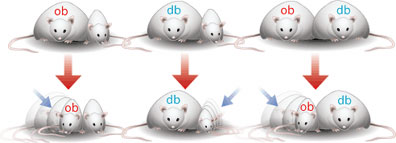
- Found that there was a "satiety factor" circulating in the blood. Hypothesized that db mice lacked the receptor to the factor, while ob mice did not produce it.
- It could not be extracted from the blood because it was present in tiny amounts. However, the gene responsible for it was eventually isolated and the "satiety factor", leptin, was produced in a lab. The leptin gene is spliced into bacteria and the bacteria sets to work producing the protein.
- By the mid 1990s it was greeted as a possible miracle cure for the rising obesity epidemic. 1995 New York Times headline read: "Researchers find hormone causes a loss of weight". Leptin is discussed as a "magic bullet", which would hopefully "change the image of obesity, helping people to see it not as a punishment for gluttony but rather as a metabolic disorder, treatable with a remedial hormone just as diabetes is treated with insulin."
- By the end of 90s none of the new research had panned out. All experiments that had been done on obese humans had found that leptin rarely caused weight loss, and if it did it was only temporary. New York Times headline from 1999 read: "Hormone that slimmed fat mice disappoints as panacea in people". Researchers determined that obese people were somehow resistant to leptin, so it was not effective in their brain.
- Since then most research has focused on understanding the metabolic pathways of leptin, and little thought has been given as to how it might be used as a treatment for obesity.
- Hypothalamus is the main organ involved in regulation of appetite; specifically the arcuate nucleus (situated at the base).
- The neurons involved primarily employ serotonin as a neurotransmitter, although neuropeptide Y and Agouti-Related peptide are also involved.
- The hypothalamus uses Ghrelin, Leptin, Insulin and PYY as markers to influence how hungry we feel.
- Ghrelin is excreted by the stomach may also be produced in the brain. Causes feelings of hunger and is associated with regular meal times. Ghrelin levels rise immediately before a meal and fall sharply after eating.
- Ghrelin Factoids: Those suffering from anorexia nervosa have higher blood levels of ghrelin. - Individuals who have undergone gastric bypass surgery produce less ghrelin. - Ghrelin acts not only on neurons in the arcuate nucleus but also activates reward circuitry in the brain associated with dopamine.

- Leptin is mainly produced by white adipose tissue. Leptin blood level is proportional to body fat. The more body fat on the body the more leptin that is produced.
- When leptin is given to genetically obese mice they lose 30% of their body weight in 2 weeks. When leptin is given to lean mice they lost all their body fat in 4 days.
- Human trials with leptin were unsuccessful. Except at the highest doses (several tablespoons a day) there were no significant changes in weight.
- Why was it so unsuccesful? Obese humans develop a resistancy to leptin in their brain.
- Umut Ozcan - Harvard - Endoplasmic Reticulum Stress Plays a Central Role in Development of Leptin Resistance
- General Hypothesis: The hypothalamus has become resistant to leptin through a process called Endoplasmic Reticulum Stress (ER Stress) which ultimately results in reduced ER function. This causes reduced function of Leptin Receptor signaling. To resensitize the brain to leptin it is necessary to improve function in the ER. Chemical chaperones have been shown to do this.

- The Endoplasmic Reticulum is an organelle responsible for protein folding and transportation of proteins to the cell membrane.
- If the normal processes of the ER are disturbed misfolded proteins accumulate in the cell. This activates cellular stress mechanism called the Unfolded Protein Response (UPR) is activated.
- UPR halts protein translation and causes an increase in the production of molecular chaperones involved in protein folding. If this mechanism is unsuccessful, UPR leads to apoptosis.
- How ER stress is induced and how this leads to UPR is not well understood. The main theory suggests that increased levels of circulating cytokines, fatty acids, excess nutrition and activation of the rapamycin pathway (involved in cellular homeostasis) contribute.
- What they demonstrated in the paper:
- Leptin Acts on a Subset of Hypothalamic neurons
- ER Stress Inhibits Leptin Receptor Signaling
- ER Stress Creates Leptin Resistance in the Brain of Lean Mice
- Improvement of ER Function Enhances Leptin Signaling
- ER Capacity of the Brain Links Obesity to Leptin Resistance
- Chemical Chaperones are Leptin Sensitizers.
2. ER Stress Inhibits Leptin Receptor Signaling
- Cells that presented the Leptin Receptor (LepRB) were exposed to tunicamycin (a chemical that induces ER stress) and then treated with leptin for 45 minutes.
- There was no evidence of leptin-stimulated tyrosine phosphorylation of LepRB or Stat3 phosphorylation (both cellular events that occur as a result of leptin binding to LepRB).

 This indicates that UPR inhibits LepRB signaling at all steps.
This indicates that UPR inhibits LepRB signaling at all steps.
- Since LepRB is folded in the ER they next investigated ER stress blocks LepRB translocation from the ER to the cell membrane as a possible explanation of the block in leptin signaling.
- They induced ER stress in cells using tunicamycin and then used immunflorescence staining to analyze LepRB levels in the cell membrane. They found that ER stress does not decrease LepRB translocation to the membrane nor does it cause a misfolding of LepRB.

3. ER Stress Creates Leptin Resistance in the Brain of Lean Mice
- First - Showed that injecting tunicamycin into the hypothalamus of lean mice caused ER Stress.
- Second - Showed that ER stress in the brain's of lean mice completely blocked activation of Stat3.

- Third - Noted that the food uptake of lean mice with induced ER stress in the hypothalamuc increased.

- Bred XNKO mice that produced less of the regulators involved in protein folding in the ER therefore making them more susceptible to ER stress (deletion of the XPB1 gene).
- On a normal diet they had a slightly lower body weight. Blood glucose and leptin levels were normal. Glucose homeostasis was maintained within a normal range.
- On a high fat diet the XNKO mice gained weight more quickly. A sharp increase in leptin level was maintained through out the experiment. They consumed more food, had a higher total fat amount and a significantly lower lean mass.


- These results support the hypothesis that ER capacity of the brain is involved in regulating body weight, leptin sensitivity and metabolic homeostasis.
- Chemical chaperones are compounds that have been found to increase ER function and decrease the accumulation of misfolded proteins in the ER, thereby reducing the likelihood that ER stress will occur.
- 2 FDA approved chemical chaperones for humans are 4-phenyl butyrate (PBA) and tauroursodeoxycholic acid (TUDCA). Past studies have shown that these chemicals can relieve ER stress in the liver and adipose tissues, as well as enhancing insulin sensitivity in mouse models.
- Attempted to reverse ER stress in the hypothalamus of mice who had been on a high fat diet. Normal mice were kept on a high-fat diet for 25 weeks and then treated with PBA for 10 days, followed by daily leptin administration.
- Control mice rapidly lost weight and then rapidly regained it. Mice treated with PBA rapidly loss weight, they also consumed less food.


- Similar results were obtained with TUDCA.
- Both PBA and TUDCA also had some success in increasing leptin sensitivity in genetically obese mice (ob/ob mice).
- After years of searching for leptin-sensitizing agents, chemical chaperones have been identified as potential novel treatment options for obesity.
hahahhaa
ReplyDeleterealisitc like it 100 times ....very very good